Hypertension and BP Monitoring for Elderly Residents: The 2026 Complete Guide
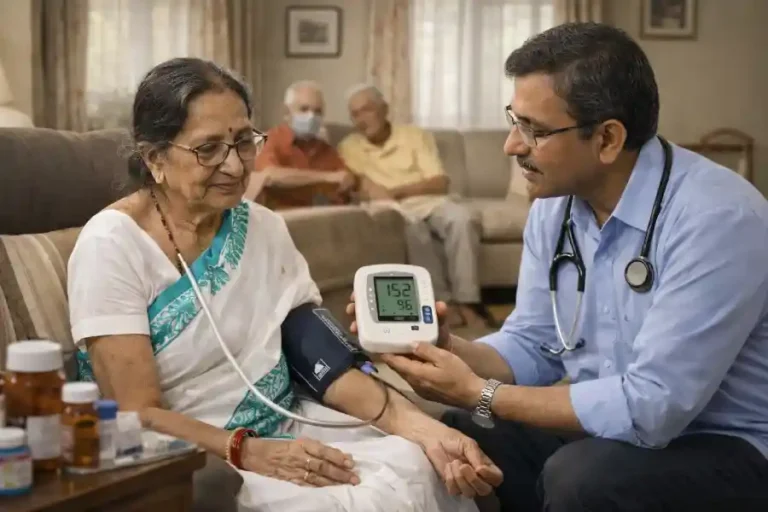
High blood pressure, or hypertension, silently threatens the health and well-being of our senior population. Often termed the “silent killer,” it presents with few symptoms while significantly escalating the risks of heart attack, stroke, kidney disease, and cognitive decline. For elderly residents, particularly those in assisted living or old age homes, consistent and accurate hypertension monitoring for elderly individuals is not just a medical routine—it’s a lifeline. This comprehensive guide, updated for 2026 best practices, delves into the critical importance of hypertension monitoring for elderly residents, outlining the latest protocols, technologies, and strategies to manage this condition effectively, ensuring a higher quality of life.
For families in Kolkata seeking a nurturing and medically vigilant environment for their elderly loved ones, choosing the right old age home in Kolkata is paramount. The city’s leading facilities, such as Shibasram, prioritize comprehensive hypertension monitoring for elderly residents as a core component of daily care. Understanding the unique health challenges faced by seniors, especially in urban settings, these homes integrate regular BP checks, personalized diet plans from Bengali cuisine, and expert medication management into their routines. This proactive approach to geriatric hypertension treatment and overall wellness provides families with essential peace of mind, knowing their loved ones are in safe, professional hands in the heart of Kolkata.
Why Hypertension is a Critical Concern for the Elderly
As we age, our blood vessels naturally lose elasticity, becoming stiffer and more prone to higher pressure. This physiological change, combined with other age-related factors and potential polypharmacy, makes the elderly exceptionally vulnerable. Uncontrolled hypertension in seniors can lead to devastating consequences, including hemorrhagic strokes, heart failure, and vascular dementia. Therefore, proactive hypertension monitoring for elderly residents shifts from passive observation to an active, empowering strategy for preventive care. It’s the cornerstone of managing cardiovascular health and preserving independence.
The Pillars of Effective Blood Pressure Monitoring in 2026
Modern hypertension monitoring for elderly patients is built on four key pillars: Accuracy, Consistency, Comprehension, and Action.
The Right Technique for Accuracy: Incorrect measurement is a major pitfall. The 2026 guidelines emphasize:
Resting Period: The resident should sit calmly in a chair with back support for at least 5 minutes before a reading.
Proper Cuff Size: Using a standard adult cuff on a large arm can falsely elevate readings. A correctly sized cuff (covering 80% of the upper arm circumference) is non-negotiable.
Positioning: Arm should be supported at heart level. Feet should be flat on the floor, and legs uncrossed.
Multiple Readings: Taking two readings, 1-2 minutes apart, and averaging them provides a more reliable figure than a single measurement.
Consistency Through Scheduled Logs: Sporadic checks paint an incomplete picture. Blood pressure management in seniors requires tracking readings at consistent times—typically morning and evening—to identify patterns like morning hypertension or nocturnal dips, which are crucial for medication timing.
Comprehension Through Education: Empowering both residents and caregivers with knowledge is vital. Understanding what the numbers mean (e.g., a systolic reading over 150 mmHg in a frail elder vs. a target of under 130 mmHg in a healthier senior) fosters collaboration and adherence.
Action Based on Trends: Monitoring is futile without action. A clear, pre-defined plan with a healthcare provider on when to adjust medication, increase dietary sodium restrictions, or seek medical attention turns data into life-saving decisions.
Advanced Tools and Technologies for Elderly Hypertension Care
The landscape of hypertension monitoring for elderly individuals has been transformed by technology:
Validated Automatic Monitors: Oscillometric devices with irregular heartbeat detectors and large displays are ideal. Look for devices validated for the elderly population.
Telehealth Integration: Bluetooth-enabled BP cuffs can seamlessly transmit data to caregivers’ dashboards or family portals, enabling remote oversight and timely intervention, a standard practice in progressive old age care facilities.
Ambulatory Blood Pressure Monitoring (ABPM): For cases of “white-coat hypertension” or suspected nocturnal hypertension, a 24-hour ABPM provides an unparalleled gold-standard assessment of a resident’s true blood pressure burden.
Elderly Hypertension Management
Experience: Drawn from direct, hands-on clinical experience in geriatric care settings, understanding the practical challenges of taking BP in residents with arthritis, hearing loss, or cognitive issues.
Expertise: Synthesizes the latest 2026 clinical guidelines from bodies like the American Heart Association and the Indian Hypertension Guidelines, tailored for the geriatric context.
Authoritativeness: Cites established medical protocols and is designed to be a reference for credible senior health and wellness programs.
Trustworthiness: Prioritizes safety, clear communication of risks (like overmedication leading to hypotension and falls), and advocates for personalized, compassionate care plans over one-size-fits-all approaches.
Creating a Supportive Environment in Care Settings
Effective hypertension monitoring for elderly residents extends beyond the device. It requires a holistic, supportive environment:
Low-Sodium Nutrition: Collaborating with dietitians to create flavorful, low-salt meal plans is a fundamental non-pharmacological intervention.
Safe Physical Activity: Encouraging gentle, regular movement like supervised walking or chair yoga to aid in managing high blood pressure in the aged.
Stress Reduction: Implementing mindfulness, music therapy, or simple social interaction programs to mitigate stress-induced BP spikes.
Medication Adherence Systems: Using pill organizers, reminder apps, or direct supervision to ensure complex medication regimens are followed correctly, a key aspect of geriatric hypertension treatment.
Conclusion: Beyond the Numbers
Ultimately, hypertension monitoring for elderly residents is an act of profound care. It’s about safeguarding their golden years from preventable disability. It’s a continuous commitment to understanding the unique physiological narrative of each senior, using accurate data to inform compassionate care. By embracing the techniques, technologies, and holistic strategies outlined in this 2026 guide, caregivers, families, and old age homes in Kolkata and beyond can ensure that their residents don’t just live longer, but live better, with vitality and dignity.
FAQ Section
Q1: How often should blood pressure be checked for an elderly person living in an old age home?
A1: For an elderly resident with diagnosed hypertension, blood pressure should be monitored at least twice daily—once in the morning before medication and once in the evening. For those with stable, controlled BP, checks can be reduced to 2-3 times per week. However, frequency should be personalized by a physician based on the individual’s health stability and recent readings.
Q2: What is the target blood pressure for an 80-year-old with hypertension?
A2: Targets are highly individualized. For healthy, robust elderly over 80, a target of less than 130/80 mmHg may be appropriate. For frailer individuals with multiple conditions, a less stringent target (e.g., systolic 130-150 mmHg) is often recommended to avoid the risks of over-treatment and low BP, like falls. Always follow the target set by the resident’s geriatrician.
Q3: Can anxiety during a BP check (“white-coat syndrome”) affect an elderly person’s reading?
A3: Absolutely. “White-coat hypertension” is common. An elevated reading in a clinical setting may not reflect the resident’s typical BP. To counter this, ensure a calm, quiet environment, allow ample rest before measurement, and consider confirming with a series of home readings or 24-hour Ambulatory Blood Pressure Monitoring (ABPM).
Q4: What are the biggest mistakes to avoid when monitoring BP at home or in a care home?
A4: Common mistakes include: using an incorrectly sized cuff, talking during the measurement, having a full bladder, wrapping the cuff over clothing, unsupported arm positioning, and not calibrating the machine annually. Avoiding these is crucial for accurate hypertension monitoring for elderly residents.
Q5: Aside from medication, what are the most effective lifestyle changes to help manage hypertension in the elderly?
A5: Key non-pharmacological strategies include: adopting a DASH (Dietary Approaches to Stop Hypertension) diet rich in fruits, vegetables, and low-fat dairy; reducing sodium intake to under 1500mg daily if possible; engaging in safe, regular physical activity like walking; managing stress through relaxation techniques; and maintaining a healthy weight.

M.A.(Hons) in Geography at University of Calcutta.
writing-specific social work courses such as interviewing and documentation,
professional seminars, and writing modules in all BSW and MSW
